ONC Health IT Certification Program Updates *Important Deadline Coming Up: December 31, 2022 The Promoting Interoperability Program started in 2011 with requiring certain clinical data be captured electronically, which including providing functionality so that patients could receive electronic copies of their health records (Stage 1). In Stage 2, there was a requirement to provide Meaningful […]
Category: COMPLIANCE
Health Plan Audits: Penalties & Risks
If wrong-doing is identified, based on health plan audits or evaluation of information, the company and company’s officials could face certain penalties, fines, and risks. The penalties and fines will be based on the type of offense, how egregious the offense is, how long it has been going on, how much harm it has done […]
Health Plan Audits: Access into Systems
Health plans can gain access into the company’s system. This will depend on what is in the company’s contract/Agreement with the health plan.
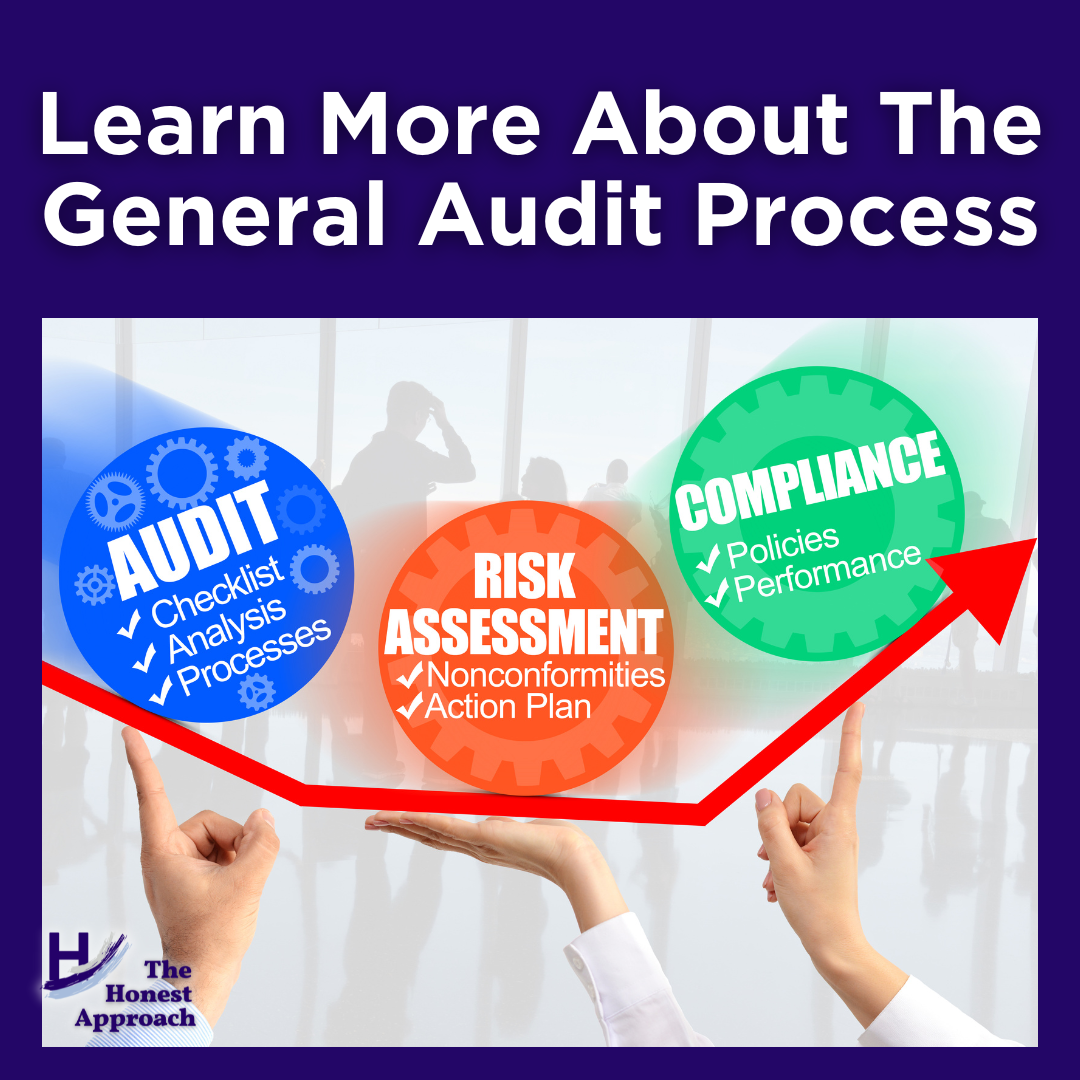
Highlights of the General Audit Process
Typically, a letter announcing the intention of an audit is sent to the company. However, I have experienced where State Agents came directly into a clinic and started the investigation immediately on premises. In this case, the investigation was based on a complaint issued to the State Medicaid agency. Having Federal and State Agents come […]
Ways a Health Plan Audit Can Be Initiated
There are several ways that a Health Plan audit can be initiated: As a result of pre-delegation audit and annual audit findings From a delegation/contractual standpoint, there can be Key Performance Indicators (KPIs) that must be met for a health plan to remain in compliance with the Centers for Medicare and Medicaid Services (CMS). For […]
Customers Perceive Shortfall in Medicare Advantage Plan Coverage of Mental Health and Substance Abuse Services, J.D. Power Finds
August 19, 2022
This is an interesting in article, just published yesterday from JD Power regarding Medicare Advantage (MA) plans and mental health coverage.
According to the study conducted by JD Power, patient satisfaction with MA plans has increased in the last year, however, patients have indicated that there is inadequate coverage for mental health and substance use disorders. The senior population has been significantly affected by the pandemic (loneliness, isolation), including many aspects around Social Determinants of Health (SDOH) such as Community, Safety & Social Context (e.g., social integration, support systems, community engagement) and Health Care System (e.g., health coverage, access/availability, and quality of care).
When Utilizing Offshore Companies, Be Sure The Highest Standards of HIPAA Privacy and Security Are In place
July 7, 2022
CEO of Raleigh Healthcare Company Pleads Guilty to Multi-Million Dollar Healthcare Fraud
The OIG has become more sophisticated in their detection and fight against fraudulent schemes.
July 6, 2022
In an interview with Health Care Compliance Association (HCCA), the new Inspector General of HHS-OIG, Christi A. Grimm indicated that their focus continues to be around compliance and fraud, waste, and abuse.
Investigation Into MA Organizations
June 30, 2022
The American Hospital Association has asked the Department of Justice (DOJ) and Centers for Medicare & Medicaid Services (CMS) to look into commercial payers that routinely deny access to care and services.
DOJ Reaches $22.7 Million Settlement with Providence Over Medically Unnecessary Neurosurgery Procedures
Thomas Sullivan Last Updated May 30, 2022
The Department of Justice had a $22.7 million settle with Providence Health & Services Washington (Providence) to resolve allegations that Providence inappropriately billed claims to federal programs (Medicare, Medicaid, Tricare, etc.) for services that were not medically necessary.